Business interests,
Banks interests,
Retail interests,
Industry interests,
Mining interests,
Economic interests,
Governments interests,
Department interests,
Companies interests.
but who is governing for yours or my bloody interests?
Always ask in whose interest?
But, to do so YOU must be interested,
Sure, be disaffected, disappointed,
hold them in disdain, or wish they were all arrested,
but you cannot afford disinterest.
Open your eyes, your ears, your heart and your mind,
look beyond the impress of main stream press,
you might just find that there is plenty of interest,
in whose interests
are being served, by those who proclaim an interest
in your interests,
while making interest
out of your disinterest.
Show your distress, make a noise,
write an email, a letter or post,
stand up, hit the street, protest.
Never lose sight, of yours, your mates,
your neighbours, your communities interests.
Think,take time, give time, help redress,
the imbalance of interests.
Deciding who will govern best,
before you cast your vote, put it through this test.
Whose interests,
will they serve best?
Then take your vote, and invest
in those that will serve the whole of your communities interests,
not just the narrow power or profit interests
of those who previously made their interest
out of your disinterest.
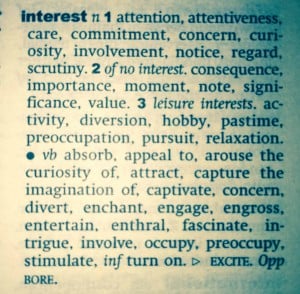
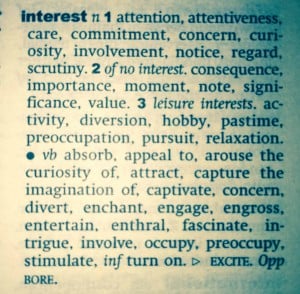
Be interested in interests!